Last Updated on April 17, 2024 by Silvy
Understanding How Common Skincare Products Can Trigger Allergic Contact Dermatitis
Have you ever experienced a frustrating flare-up after introducing a new, luxurious face cream into your routine?
Itchy, red patches, burning, and uncomfortable tightness – these are all signs of a potential allergic contact dermatitis (ACD) reaction. While we spend a lot of time researching the benefits of various skincare ingredients, understanding the potential downsides is equally important.
In this comprehensive guide, we’ll delve into the world of ACD and skincare products, uncovering the culprits, explaining the science behind the reaction, and equipping you with knowledge to navigate the world of beauty products with confidence.
This guide will serve as your ultimate defense shield against unwanted skin flare-ups. So, buckle up, skincare enthusiasts, and get ready to transform from a confused consumer to a dermatitis-detecting extraordinaire!
Here’s a sneak peek of what we’ll cover:
- What is Allergic Contact Dermatitis (ACD) and How Does it Differ from Irritant Contact Dermatitis?
- The Sneaky Culprits: Common Skincare Ingredients that Trigger ACD
- The Plot Thickens: Unveiling the Scientific Underbelly of ACD
- Identifying the Enemy: Patch Testing – Your Weapon of Choice
- Taming the Beast: Soothing and Treating ACD Symptoms
- Prevention is Key: Practical Tips to Minimize the Risk of ACD
- Beyond the Basics: ACD in Different Skin Types and Conditions
- Living with ACD: When Skincare Becomes a Balancing Act
- The Final Showdown: Can You Completely Avoid ACD Triggers?
- Frequently Asked Questions (FAQs) about ACD and Skincare Products
This in-depth exploration will empower you to make informed choices about the products you use, ensuring a healthy and radiant complexion.
Remember, beautiful skin starts with knowledge, and by understanding ACD, you’re taking control of your skincare journey.
Let’s dive deeper!

What is Allergic Contact Dermatitis (ACD) and How Does it Differ from Irritant Contact Dermatitis?
Imagine your skin as a magnificent fortress protecting your inner sanctum. ACD is like a Trojan horse, appearing harmless at first, but unleashing an inflammatory response within the walls.
This allergic reaction occurs when your immune system identifies a specific ingredient in a skincare product as a threat.
It’s crucial to distinguish ACD from its close cousin, irritant contact dermatitis (ICD). ICD is a non-immunological reaction where a product irritates the skin, causing redness, dryness, or burning.
Unlike ACD, which develops over time with repeated exposure, ICD can occur with the very first use of a product, especially if it’s harsh or contains strong fragrances.
Understanding this difference is key to tackling skin woes effectively. We’ll explore the science behind ACD in the next section, but for now, let’s focus on the common culprits lurking in your favorite skincare products.
Our quest to achieve flawless skin often leads us down a path lined with countless products, each boasting unique benefits.
However, some of these seemingly innocuous ingredients can be the secret villains behind an ACD flare-up. Here are some of the most common offenders:
- Fragrances: Ever noticed a generic “fragrance” listed on the ingredient label? This term can encompass a complex blend of thousands of chemicals, any of which could trigger an allergic reaction.
- Preservatives: Essential for extending product shelf life, preservatives like formaldehyde, parabens, and isothiazolinones can sometimes be problematic, especially for those with sensitive skin.
- Metals: Nickel, chromium, and cobalt, commonly found in sunscreens and cosmetics, can cause itchy, red rashes.
- Lanolin: Derived from sheep’s wool, lanolin is a popular moisturizing ingredient, but it can trigger allergies in some individuals.
- Sunscreen ingredients: Oxybenzone and octinoxate, while effective at sun protection, can be culprits behind ACD, particularly for those with eczema-prone skin.
- Essential oils: Though touted for their natural benefits, essential oils like tea tree oil, lavender oil, and citrus oils can cause allergic reactions when applied topically.
- Acids: While alpha hydroxy acids (AHAs) and beta hydroxy acids (BHAs) are hailed for their exfoliating properties, they can be irritating and trigger ACD in individuals with sensitive skin.
- Alcohol: Used as a solvent and astringent, alcohol can be drying and exacerbate ACD symptoms.
- Color additives: Dyes and pigments used in makeup and skincare products can sometimes trigger allergic reactions.
- Botanical extracts: While plant-based ingredients are generally considered gentle, some extracts, like witch hazel or aloe vera, can cause ACD in some people.
It’s important to remember that this list is not exhaustive. Any ingredient in a skincare product has the potential to trigger ACD in susceptible individuals.
The key takeaway? Pay close attention to ingredient labels and be mindful of introducing new products one at a time to identify potential triggers.
In the next section, we’ll delve into the fascinating science behind ACD, unveiling the intricate dance between your immune system and those pesky skincare ingredients.

The Plot Thickens: Unveiling the Scientific Underbelly of ACD
Imagine your skin as a sophisticated security system. When a foreign object, like a skincare ingredient, breaches the outer layer (stratum corneum), specialized sentinel cells called Langerhans cells spring into action.
These cells capture the “invader” and present it to T-lymphocytes, the body’s immune system soldiers.
The First Encounter: During the initial exposure, the T-lymphocytes become “sensitized” to the specific ingredient. They don’t launch a full-scale attack just yet, but they create a memory of the invader.
The Sneak Attack: Now, upon subsequent exposures to the same ingredient, the “sensitized” T-lymphocytes recognize it as a threat.
They trigger an inflammatory response, releasing a cascade of chemicals that cause the classic signs of ACD: redness, itching, burning, and swelling. This is the battle raging beneath the surface of your skin, leading to the uncomfortable flare-up.
The Inflammatory Cascade: The released chemicals include cytokines, which attract other immune cells to the site, further amplifying the inflammation.
Additionally, histamine, a potent chemical, is released, causing itching and swelling. This intricate web of reactions is what manifests as the visible symptoms of ACD.
Understanding this immunological dance can empower you to:
- Be patient: ACD reactions develop over time with repeated exposure. Identifying the culprit might take some trial and error.
- Recognize the signs: Itchiness is often a telltale sign of ACD, as opposed to burning, which might be more indicative of irritation.
In the next section, we’ll equip you with your ultimate weapon against ACD – the power of patch testing!

Identifying the Enemy: Patch Testing – Your Weapon of Choice
Imagine a world where you can identify potential skincare triggers before they unleash havoc on your face.
Enter the hero of this story – patch testing. This simple yet effective technique allows you to proactively discover ingredients that might cause ACD.
Here’s how you can become a patch testing pro:
Gather Your Arsenal:
- Patch test kit: You can purchase commercially available patch test kits containing common allergens found in skincare products. Alternatively, consult a dermatologist who can perform a more comprehensive patch test with a wider range of ingredients.
- Distilled water: This will be used to dilute harsher ingredients before application.
- Cotton swabs: These will be your tools for applying the product samples.
- Bandages: Secure the patch test applications to prevent them from dislodging.
- Journal: Meticulously record the tested products and any observed reactions.
The Battle Plan:
- Cleanse and dry a small area on your upper back (an area less likely to be irritated by clothing).
- Apply a small amount of the product you want to test (dilute harsher ingredients with distilled water) to the designated area using a cotton swab.
- Label the patch clearly with the product name.
- Secure the patch with a bandage.
- Repeat steps 1-4 for each product you want to test, ensuring there’s enough space between patches to avoid overlap.
- Leave the patches untouched for 48 hours.
- Remove the patches and meticulously examine the test sites for any redness, itching, bumps, or swelling. Even a faint reaction can indicate ACD.
- Record your observations in your journal, noting the product and any reactions observed.
Remember: Patch testing is a diagnostic tool, not a foolproof shield. It’s crucial to interpret the results with caution. If you experience a significant reaction, discontinue use of the product and consult a dermatologist for further guidance.
In the next section, we’ll explore strategies to soothe and manage ACD symptoms after encountering a trigger.
Taming the Beast: Soothing and Treating ACD Symptoms
So, you’ve identified the culprit behind your ACD flare-up. Now what? Don’t fret, for there are ways to calm the inflammatory storm and restore your skin’s serenity.
Here are some effective strategies to manage ACD symptoms:
1. Elimination is Key: The most crucial step is to completely eliminate the offending ingredient from your skincare routine. This might involve decluttering your product stash and carefully scrutinizing labels of new purchases.
2. Gentle Cleansing: Opt for fragrance-free, gentle cleansers to remove any residual traces of the triggering ingredient and soothe irritated skin. Look for cleansers formulated with calming ingredients like colloidal oatmeal or ceramides.
3. Cool Compresses: Apply cool compresses soaked in distilled water to the affected area for 10-15 minutes at a time, several times a day. This helps reduce inflammation and alleviate itching.
4. Moisturize Wisely: Hydration is essential for restoring skin barrier function. Choose fragrance-free, hypoallergenic moisturizers formulated for sensitive skin. Look for ingredients like hyaluronic acid or ceramides to replenish moisture and strengthen the skin’s barrier.
5. Topical Steroids: In some cases, a dermatologist might prescribe topical corticosteroids to reduce inflammation and itching more effectively. Follow the prescribed regimen meticulously and don’t self-medicate with corticosteroids.
6. Resist the Itch: Scratching can worsen the flare-up. Applying a cold compress or using a fragrance-free lotion can help alleviate the urge to scratch. Consider wearing loose-fitting clothing to avoid further irritation.
7. Patience is a Virtue: Healing takes time. While relief might be noticeable within a few days, complete resolution of ACD symptoms might take several weeks. Be patient and consistent with your skincare routine.
Remember: If your symptoms are severe or don’t respond to at-home treatments, consult a dermatologist for a personalized treatment plan.
By following these strategies, you can effectively manage ACD symptoms and prevent future flare-ups. In the next section, we’ll delve into preventative measures to minimize the risk of ACD altogether.
Prevention is Key: Practical Tips to Minimize the Risk of ACD
An ounce of prevention is worth a pound of cure, as the saying goes. Here are some proactive steps you can take to minimize the risk of ACD flare-ups:
-
Read Labels Religiously: Become a label-reading detective! Scrutinize ingredient lists and familiarize yourself with common allergens. Pay particular attention to broad terms like “fragrance” which can encompass a multitude of potential triggers.
-
Introduce Products Slowly: Don’t overwhelm your skin! Introduce new products one at a time, allowing a week or two for your skin to adjust before incorporating another. This helps pinpoint the culprit if an ACD reaction occurs.
-
Patch Test When in Doubt: If you’re unsure about a new product, especially if it contains a plethora of ingredients, patch test it before applying it liberally to your face. Patch testing, as discussed earlier, is a powerful tool for proactive identification of potential triggers.
-
Less is More: A streamlined skincare routine is often kinder to sensitive skin. Stick to the essentials: cleanser, moisturizer, and sunscreen. Avoid layering too many products at once, which can overwhelm the skin barrier.
-
Natural Doesn’t Always Mean Safe: Don’t be fooled by the “natural” label. Even natural ingredients like essential oils or botanical extracts can trigger ACD in some individuals. Patch testing is crucial regardless of the product’s labeling.
-
Consult a Dermatologist: If you have a history of allergies or sensitive skin, consider consulting a dermatologist for personalized guidance on navigating the world of skincare products. They can recommend suitable products and perform comprehensive patch testing to identify potential triggers.
By incorporating these preventative measures into your skincare routine, you can significantly reduce your risk of encountering ACD flare-ups. In the next section, we’ll explore how ACD can manifest differently in various skin types and conditions.
Beyond the Basics: ACD in Different Skin Types and Conditions
While ACD can affect anyone, some skin types and conditions might be more susceptible or experience unique presentations. Here’s a closer look:
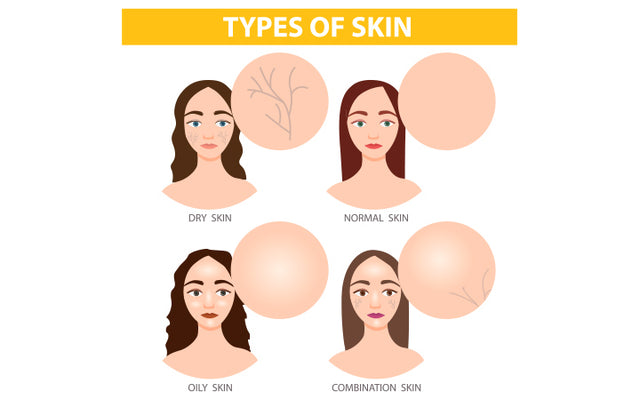
- Sensitive Skin: Individuals with inherently sensitive skin are more prone to ACD reactions due to a compromised skin barrier. They might experience a heightened reaction to even low concentrations of triggering ingredients.
- Dry Skin: Dry skin often lacks a robust barrier, making it more vulnerable to irritants and allergens. ACD in dry skin can manifest as intense dryness, scaling, and even cracking.
- Oily Skin: While oily skin tends to be more resilient, it’s not invincible. ACD in oily skin might present as breakouts, increased oil production, or a combination of both.
- Eczema: People with eczema, a chronic inflammatory skin condition, often have a weakened skin barrier, making them more susceptible to ACD flare-ups. ACD in eczema can exacerbate existing symptoms like itching, redness, and flaking.
- Rosacea: Rosacea, a condition characterized by facial redness and inflammation, can be triggered by certain skincare ingredients. ACD in rosacea can worsen existing symptoms and lead to increased flushing and sensitivity.
Understanding how ACD manifests in different skin types and conditions allows for:
- Tailored Skincare Routine: Developing a skincare routine that caters to your specific skin type and any underlying conditions can minimize the risk of ACD.
- Targeted Treatment: If you experience ACD alongside another skin condition, consulting a dermatologist can lead to a more targeted treatment approach to address both issues.
In the next section, we’ll delve into the realities of living with ACD and offer strategies for navigating the world of skincare products when faced with this challenge.

Living with ACD: When Skincare Becomes a Balancing Act
Living with ACD can feel like navigating a minefield of potential triggers. However, with the right approach and a dash of patience, you can create a beautiful skincare routine that works for you.
Here are some tips for living well with ACD:
-
Embrace Minimalism: A streamlined skincare routine is often your best friend. Focus on gentle, fragrance-free products formulated for sensitive skin. Look for ingredients known to soothe and strengthen the skin barrier, like ceramides and hyaluronic acid.
-
Patch Testing Becomes Your BFF: Develop a fondness for patch testing! Consider patch testing any new product, even those marketed for sensitive skin. Remember, “natural” doesn’t always equate to safe for ACD-prone individuals.
-
Befriend a Dermatologist: Dermatologists are your allies in the battle against ACD. They can offer personalized guidance, recommend suitable products, and perform comprehensive patch testing to identify a wider range of potential triggers.
-
Patience is Key: Healing from ACD flare-ups and identifying triggers takes time. Be patient with your skin and consistent with your skincare routine. Don’t get discouraged if results aren’t instantaneous.
-
Listen to Your Skin: Your skin is your best communicator. Pay attention to how it reacts to different products and environments. Avoid anything that triggers itching, burning, or redness.
-
Makeup Maneuvers: Makeup lovers with ACD can rejoice! Look for mineral makeup free of fragrance, dyes, and common allergens. Patch test makeup products meticulously before applying them to your entire face.
-
Join the ACD Community: Connect with others who understand the challenges of ACD. Online forums and support groups can be a valuable source of information, shared experiences, and emotional support.
Living with ACD doesn’t have to mean sacrificing beautiful skin. By adopting these strategies and embracing a mindful approach, you can create a skincare routine that keeps your skin healthy and radiant.
In the next section, we’ll tackle some frequently asked questions (FAQs) about ACD and skincare products, empowering you with even more knowledge to navigate this topic confidently.
Frequently Asked Questions (FAQs) about ACD and Skincare Products
Can I develop ACD to an ingredient I’ve used for years without any problems?
Yes, ACD can develop over time with repeated exposure. The initial exposures might not trigger a reaction, but your immune system can become sensitized to the ingredient, leading to a reaction upon subsequent exposures.
How long does it take for ACD symptoms to resolve?
The duration of ACD symptoms depends on the severity of the reaction and the effectiveness of treatment. Mild flare-ups might resolve within a few days with proper care, while more severe cases might take weeks to heal completely.
Are there any foods that can trigger ACD?
While uncommon, some individuals might experience allergic reactions to certain foods that manifest as skin irritation. This is called food-induced dermatitis. If you suspect a link between your diet and ACD flare-ups, consult a dermatologist for guidance.
Can stress trigger ACD?
Stress can exacerbate existing skin conditions, including ACD. While stress itself might not directly cause ACD, it can worsen symptoms and make you more susceptible to flare-ups. Techniques like meditation or yoga can be helpful in managing stress and potentially reducing the impact on your skin.
Is it possible to completely avoid ACD triggers?
Unfortunately, there’s no guaranteed way to avoid all potential ACD triggers. However, by following the tips outlined in this guide, including patch testing, using fragrance-free products, and maintaining a healthy skin barrier, you can significantly reduce your risk of flare-ups.
Remember, consulting a dermatologist is crucial for personalized diagnosis and management of ACD.
They can provide tailored advice and treatment plans based on your specific needs and triggers.
By understanding ACD, adopting preventative measures, and seeking professional guidance when necessary, you can embark on a journey towards healthy, beautiful skin, even with ACD.
Here are some credible sources to support the information in this article on Allergic Contact Dermatitis (ACD) and Skincare Products:
- American Academy of Dermatology Association (AAD): https://www.aad.org/member/clinical-quality/guidelines/atopic-dermatitis
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/dermatitis-eczema/symptoms-causes/syc-20352380
- National Institute of Environmental Health Sciences (NIEHS): https://www.ncbi.nlm.nih.gov/books/NBK459230/
- Journal of the American Academy of Dermatology (JAAD): https://www.jaad.org/ (This is a peer-reviewed medical journal that requires a paid subscription for full access, but the linked page offers an overview of patch testing.)
- International Fragrance Research Institute (IFRA): https://ifrafragrance.org/priorities/ingredients/ifra-transparency-list (This website provides information on potential fragrance allergens, though it’s important to note that fragrance can be a complex blend and ACD reactions can occur to unlisted ingredients.)
Remember, these are just a few resources, and it’s always recommended to consult with a licensed dermatologist for personalized diagnosis and treatment of ACD.